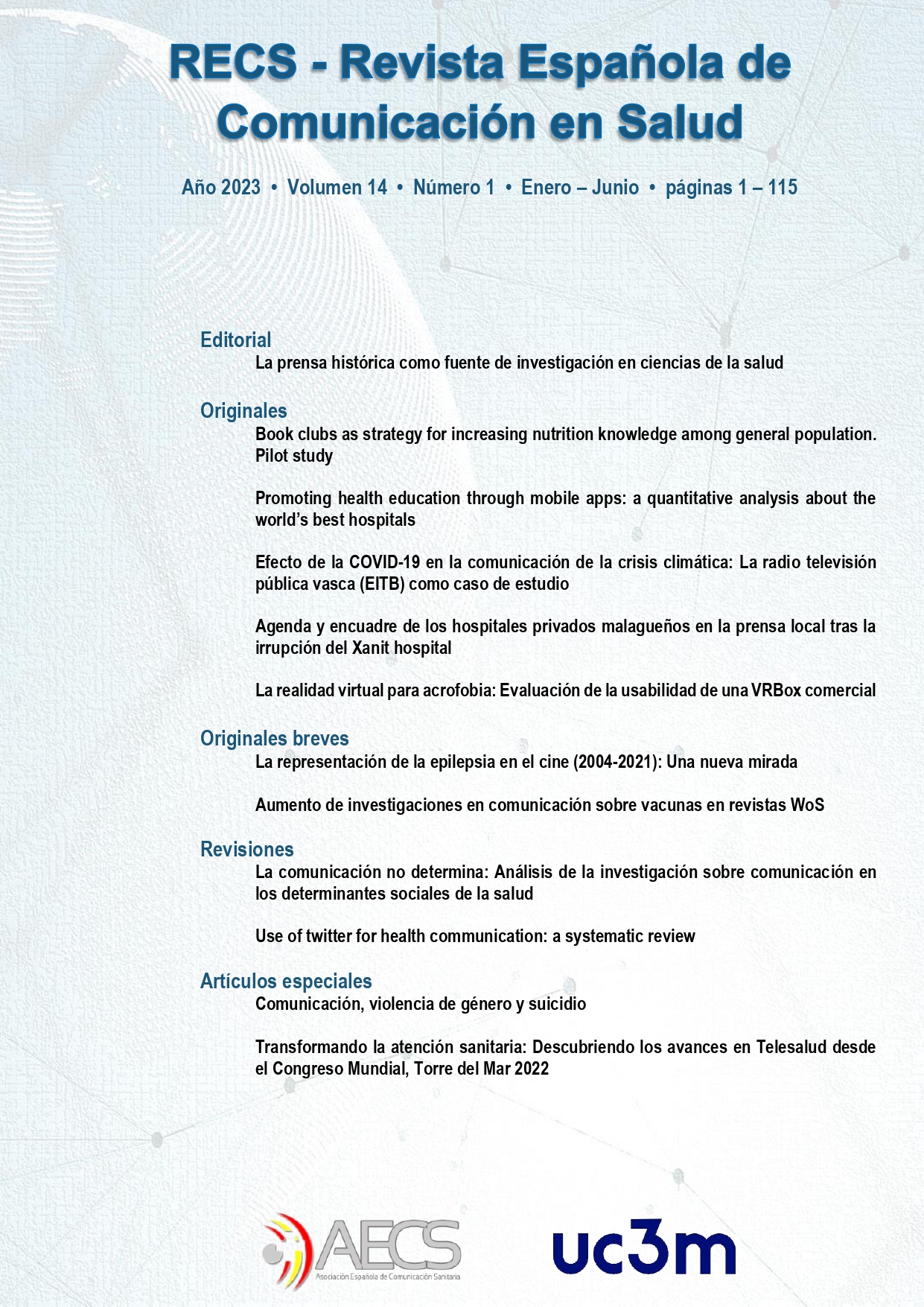
La promoción de la educación en salud a través de las mobile apps
Un estudio cuantitativo sobre los mejores hospitales del mundo
DOI:
https://doi.org/10.20318/recs.2023.7429Palabras clave:
hospitales, educación en salud, aplicaciones móviles, pacientes, enfermedades no transmisiblesResumen
Introducción: Promover la educación en salud a través de diferentes plataformas (portal del paciente, redes sociales, sitios web) se ha convertido en una práctica común en muchos países. Estos últimos años, muchos hospitales se han centrado en las aplicaciones móviles como herramienta de educación sanitaria. Objetivo: Este artículo tiene como objetivo analizar cómo deberían utilizar los hospitales las mobile apps para fomentar la educación en salud y así mejorar sus relaciones con los pacientes. Metodología: Para responder a esta pregunta, realizamos una revisión de literatura sobre educación en salud, aplicaciones móviles, empoderamiento de los pacientes y enfermedades no transmisibles; y posteriormente, recurrimos a 38 indicadores para analizar cómo los 150 mejores hospitales del mundo gestionan estas plataformas para promover la educación en salud. Conclusión: Concluimos que los tres criterios principales que los hospitales deben respetar cuando usan aplicaciones móviles con fines educativos son: 1) respetar las necesidades informativas y emocionales de los pacientes; 2) evaluar las habilidades de los profesionales de la salud y los pacientes en alfabetización móvil; y 3) considerar las prioridades de salud pública.
Descargas
Referencias
Affinito, L., Fontanella, A., Montano, N., & Brucato, A. (2022). How physicians can empower patients with digital tools: A joint study of the Italian Scientific Society of Internal Medicine (FADOI) and the European Federation of Internal Medicine (EFIM). Journal of Public Health, 30 (3). https://doi.org/10.1007/s10389-020-01370-4
Alanazi, M. (2021). Effect of patient education in family medicine practices. Multicultural Education, 7 (7). https://doi.org/10.5281/zenodo.5112133
Andelman, S., Bu, D., Debellis, N., Nwachukwu, C., Osman, N., Gladstone, J., & Colvin, A. (2019). Preoperative patient education may decrease postoperative opioid use after meniscectomy. Arthroscopy, Sports Medicine, and Rehabilitation, 2(1), e33-e38. https://doi.org/10.1016/j.asmr.2019.10.006
Ardisonne, A. (2020). Information and communication technologies and patient empowerment: A complex skein. International Journal of Medicine and Medical Sciences, 12(1), 8-17. https://doi.org/10.5897/IJMMS2020.1412
Bange, M., Huh, E., Novin, S., Hui, F., & Yi, P. (2019). Readability of patient education materials from radiologyInfo.org: has there been progress over the past 5 years? American Journal of Roentgenology, 213(4), 875-879. https://doi.org/10.2214/AJR.18.21047
Chen, C., Wang, L., Chi, H., Chen, W., & Park, M. (2020b). Comparative efficacy of social media delivered health education on glycemic control: A meta-analysis. International Journal of Nursing Sciences, 7(3), 359- 368. http://dx.doi.org/10.1016/j.ijnss.2020.04.010
Civitelli, G., Tarsitani, G., Rinaldi, A., & Marceca, M. (2020). Medical education: an Italian contribution to the discussion on global health education. Global Health, 16(1), 30. https://doi.org/10.1186/s12992-020-00561-8
Comp, G., Dyer, S., & Gottlieb, M. (2020). Is TikTok the next social media frontier for medicine? AEM Education and Training, 5(3), 10.1002/aet2.10532. https://doi.org/10.1002/aet2.10532
Doffoel, M., Tripon, S., Ernwein, F., Chaffraix, F., Haumesser, L., Bader, R., ... Baumert, T. (2022). Place of therapeutic patient education in chronic hepatitis C treated with direct-acting antivirals. Open Journal of Gastroenterology and Hepatology, 5, 60.
Driever, E., Stiggelbout, A., & Brand, P. (2019). Shared decision making: physicians’ preferred role, usual role and their perception of its key components. Patient Education and Counseling, 103. https://doi.org/10.1016/j.pec.2019.08.004
Feng, L., Wang, W., Wu, M., & Ma, H. (2021). Effect of WeChat-based health education combined with satir model on self-management behaviors and social adaptation in colorectal cancer patients during the perioperative period. Journal of Healthcare Engineering, 2701039. https://doi.org/10.1155/2021/2701039
Fittipaldi, A., O’Dwyer, G., Henriques, P. (2021). Health education in primary care: approaches and strategies envisaged in public health policies. Interface, 25, e200806. https://doi.org/10.1590/interface.200806
Hammoud, S., Amer, F., Lohner, S., & Kocsis, B. (2020). Patient education on infection control: A systematic review. American Journal of Infection Control, 48(12), 1506-1515. https://doi.org/10.1016/j.ajic.2020.05.039
Herzig Van Wees, S., & Holmer, H. (2020). Global health beyond geographical boundaries: reflections from global health education. BMJ Global Health, 5, e002583. https://doi.org/10.1136/bmjgh-2020-002583
Jamleh, A., Nassar, M., Alissa, H., & Alfadley, A. (2021). Evaluation of YouTube videos for patients’ education on periradicular surgery. PLoS ONE, 16(12), e0261309. https://doi.org/10.1371/journal.pone.0261309
Kumar, K., Balazy, K., Gutkin, P., Jacobson, C., Chen, J., Karl, J., ... Host, K. (2021). Association between patient education videos and knowledge of radiation treatment. International Journal of Radiation Oncology, Biology and Physics, 109 (5), 1165-1175. https://doi.org/10.1016/j.ijrobp.2020.11.069
Kuwabara, A., Su, S., & Krauss, J. (2019). Utilizing digital health technologies for patient education in lifestyle medicine. American Journal of Lifestyle Medicine, 14(2), 137-142. https://doi.org/10.1177/1559827619892547
Lavdaniti, M. (2020). Contemporary issues in cancer patients’ education. International Journal of Caring Sciences, 13 (1), 1-3. Lee, A., & Quinn, M. (2021). Global health education in U.K. universities. Journal of Global Health, 5(3), 155- 162. https://doi.org/10.1016/j.glohj.2021.06.001
Leemans, C., Van den Broucke, S., & Philippe, M. (2021). L’impact différentiel des dimensions de la littératie en santé sur l’adhésion au traitement des patients diabétiques. Education Thérapeutique du Patient, 13 (2), 20203. https://doi.org/10.1051/tpe/2021013
Li, W., Liao, J., Li, Q., Baskota, M., Wang, X., Tang, Y., ... COVID-19 Evidence and Recommendations Working Group. (2020). Public health education for parents during the outbreak of COVID-19: a rapid review. Annals of Translational Medicine, 8(10), 628. https://doi.org/10.21037/atm-20-3312
Lu, X., & Zhang, R. (2021). Association between eHealth literacy in online health communities and patient adherence: cross-sectional questionnaire study. Journal of Medical Internet Research, 23(9), e14908. https://doi.org/10.2196/14908
Machado, R., Turrini, R., & Sousa, C (2020). Mobile applications in surgical patient health education: an integrative review. Revista da Escola de Enfermagem da USP, 54, e03555. http://dx.doi.org/10.1590/S1980-220X2018032803555
Mateus-Coelho, N., & Avila, P (2021). Application of the industry 4.0 technologies to mobile learning and health education apps. FME Transactions, 49 (4), 877. https://doi.org/10.5937/fme2104876M
Meinert, E., Rahman, E., Potter, A., Lawrence, W., & Van Velthoven, M, (2020). Acceptability and usability of the mobile digital health app NoObesity for families and health care professionals: protocol for a feasibility study. JMIR Research Protocols, 9(7), e18068. https://doi.org/10.2196/18068
Mentrup, S., Harris, E., Gomersall, T., Köpke, S., Astin, F. (2020). Patients’ experiences of cardiovascular health education and risk communication: a qualitative synthesis. Qualitative Health Research, 30 (1), 88- 104. https://doi.org/10.1177/1049732319887949
Morsa, M. (2021). Une éthique minimale de l’éducation à l’autonomie en santé de la population adolescente vivant avec une maladie chronique. Éthique en Education et en Formation, 10, 62–76. https://doi.org/10.7202/1076820ar
Navarro, M. (2020). Patients’ empowerment and the role of patients’ education. Medical Research Archives, 8 (12). https://doi.org/10.18103/mra.v8i12.2306
Navarro Martínez, O., Igual García, J., & Traver Salcedo, V. (2021). Estimating patient empowerment and nurses’ use of digital strategies: eSurvey study. International Journal of Environmental Research and Public Health, 18(18), 9844. https://doi.org/10.3390/ijerph18189844
NewsWeek (2022). The World’s Best Hospitals 2022. Document retrieved from: https://www.newsweek.com/worlds-best-hospitals-2022
Oudkerk, M., Hooglugt, J., Schijven, M., Mulder, B., Bouma, B., Winter, R., ... Winter, M. (2021). Review of digitalized patient education in cardiology: a future ahead?. Cardiology, 146 (2). https://doi.org/146.10.1159/000512778
Palacios-Gálvez, S., Andrés-Villas, M., Vélez-Toral, M., & Merino-Godoy, Á. (2021). Nominal groups to develop a mobile application on healthy habits. Healthcare, 9, 378. https://doi.org/10.3390/healthcare9040378
Parkes, M., Poland, B., Allison, S., Cole, D., Culbert, I., Gislason, M., ... Waheed, F. (2020). Preparing for the future of public health: ecological determinants of health and the call for an eco-social approach to public health education. Canadian Journal of Public Health, 111, 60– 64. https://doi.org/10.17269/s41997-019-00263-8
Pekonen, A., Eloranta, S., Stolt, M., Virolainen, P., & Leino-Kilpi, H. (2020). Measuring patient empowerment - A systematic review. Patient Education and Counseling, 103(4), 777-787. https://doi.org/10.1016/j.pec.2019.10.019
Ratri, D., Hamidah, K., Puspitasari, A., & Farid, M (2020). Video-based health education to support insulin therapy in diabetes mellitus patients. Journal of Public Health Research, 9(2), 1849. https://doi.org/10.4081/jphr.2020.1849
Rowland, S., Fitzgerald, E., Holme, T., Powell, J., & McGregor, A. (2020). What is the clinical value of mHealth for patients? NPJ Digital Medicine, 3 (4). https://doi.org/10.1038/s41746-019-0206-x
Schulz, A., Mehdipanah, R., Chatters, L., Reyes, A., Neblett, E., & Israel, B (2020). Moving health education and behavior upstream: lessons from COVID-19 for addressing structural drivers of health inequities. Health Education Behavior, 47(4), 519- 524. https://doi.org/10.1177/1090198120929985
Shi, M., Zhang, P., Xia, L., Wei, Z., Bi, F., Xu, Y., & Wang, P. (2021). Application of multimode health education combined with humanistic care in pain management of patients with femoral fracture and its influence on VAS score. Journal of Healthcare Engineering, 1242481. https://doi.org/10.1155/2021/1242481
Simonsmeier, B., Flaig, M., Simacek, T., & Schneider, M. (2021). What sixty years of research says about the effectiveness of patient education on health: a second order meta-analysis. Health Psychology Review. 24, 1-25. https://doi.org/10.1080/17437199 .2021.1967184
Soep, S., & Agussalim, A. (2020). The impact of health education about Diabetes mellitus on patient knowledge to control their blood sugar. Journal of Advanced Pharmacy Education & Research,10(3), 141-145.
Sola Pueyo, J. de. (2022). La ciencia y los científicos como fuentes informativas de los medios: Análisis y aprendizajes de la pandemia del coronavirus. Revista Española de Comunicación en Salud, 13(1), 33-45. https://doi.org/10.20318/recs.2022.6361
Steves, S., & Scafide, K. (2021). Multimedia in preoperative patient education for adults undergoing cancer surgery: A systematic review. European Journal of Oncology Nursing, 52, 101981. https://doi.org/10.1016/j.ejon.2021.101981
Suárez-Argüello, J., Blanco-Castillo, L., Perea-Rangel, J., Villarreal-Ríos, E., Vargas-Daza, E., Galicia-Rodríguez, L., & Martínez-González, L (2021). Creencias de enfermedad, creencias de medicación y adherencia al tratamiento en pacientes con hipertensión arterial. Archivos de Cardiología de México. https://doi.org/10.24875/ACM.21000026
Świątoniowska-Lonc, N., Sławuta, A., Dudek, K., Jankowska, K., & Jankowska-Polańska, B. (2020). The impact of health education on treatment outcomes in heart failure patients. Advances in Clinical and Experimental Medicine, 29(4), 481–492. https://doi.org/10.17219/acem/115079
Tassone, C., Keshavjee, K., Paglialonga, A., Moreira, N., Pinto, J., & Quintana, Y. (2020). Evaluation of mobile apps for treatment of patients at risk of developing gestational diabetes. Health Informatics Journal, 26 (2), 146045821989663. https://doi.org/10.1177/1460458219896639
Team, V., Bouguettaya, A., Richards, C., Turnour, L., Jones, A., Teede, H., Weller, C. (2020). Patient education materials on pressure injury prevention in hospitals and health services in Victoria, Australia: Availability and content analysis. International wound journal, 17(2), 370–379. https://doi.org/10.1111/iwj.13281
Tilkin, C., De Winter, M., Ketterer, F., Etienne, A., Vanmeerbeek, M., & Schoenaers, F. (2019). Considering patients’ empowerment in chronic care management: a cross-level approach. European Journal of Investigation in Health, Psychology and Education, 10(1), 134–142. https://doi.org/10.3390/ejihpe10010012
Tomokawa, S., Shirakawa, Y., Miyake, K., Ueno, M., Koiso, T., & Asakura, T. (2021). Lessons learned from health education in Japanese schools. Pediatrics International, 63(6), 619-630. https://doi.org/10.1111/ped.14637
Troiseufs, A. (2020). Patients intervenants, médiateurs de santé-pairs: quelles figures de la pair-aidance en santé ? Rhizome, 1 (2), 27-36. https://doi.org/10.3917/rhiz.075.0027
Tuominen, L., Ritmala-Castrén, M., Nikander, P., Mäkelä, S., Vahlberg, T., & Leino-Kilpi, H. (2021). Empowering patient education on self-care activity among patients with colorectal cancer – a research protocol for a randomised trial. BMC Nursing, 20, 94. https://doi.org/10.1186/s12912-021-00617-z
Turkdogan, S., Schnitman, G., Wang, T., Gotlieb, R., How, J., & Gotlieb, W. (2021). Development of a digital patient education tool for patients with cancer during the COVID-19 pandemic. JMIR Cancer, 7(2), e23637. https://doi.org/10.2196/23637
Vaartio-Rajalin, H., Nyholm, L., & Fagerström, L. (2020). Patient education in the hospital-at-home care context. Patient Experience Journal, 7 (1), 65-74. https://doi.org/10.35680/2372-0247.1408
Van den Broucke, S. (2020). Why health promotion matters to the COVID-19 pandemic, and vice versa. Health Promotion International, 35(2), 181-186. https://doi.org/10.1093/heapro/daaa042
World Health Organization (2022). Noncommunicable diseases. Key facts. Document retrieved on 7th June 2020 from: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
Yin, Z., Lesser, J., Paiva, K., Zapata, J., Moreno-Vasquez, A., Grigsby, T., ... Wang, J. (2020). Using mobile health tools to engage rural underserved individuals in a diabetes education program in South Texas: feasibility study. JMIR Mhealth and Uhealth, 8(3), e16683. https://doi.org/10.2196/16683
Yu, C., Chao, C., Chang, C., Chen, R., Cheng, P., & Liu, Y. (2021). Exploring behavioral intention to use a mobile health education website: an extension of the UTAUT 2 Model. Sage Open. https://doi.org/10.1177/21582440211055721
Publicado
Número
Sección
Licencia
Los textos publicados en esta revista están –si no se indica lo contrario– bajo una licencia Reconocimiento-Sin obras derivadas 3.0 España de Creative Commons. Puede copiarlos, distribuirlos y comunicarlos públicamente siempre que cite su autor y la revista y la institución que los publica y no haga con ellos obras derivadas. La licencia completa se puede consultar en: http://creativecommons.org/licenses/by-nd/3.0/es/deed.es
Los derechos de autor pertenecen al autor de la obra por el mero hecho de su creación:
· Los derechos de contenido moral son irrenunciables e inalienables.
· Los derechos de contenido económico, o derechos de explotación, pueden ser cedidos a terceros como ocurre con los trabajos publicados, en los que el autor cede parte o la totalidad de estos derechos a la editorial.
El autor puede autoarchivar sus artículos en un repositorio institucional, siempre que se cite su publicación en esta revista.